Aomar Ammar-Khodja a Ismail Benkaidali a Bakar Bouadjar b Amina Serradj c Abdelhamid Titi d Hakima Benchikhi e Said Amal f Badreddine Hassam g Abdelhak Sekkat h Fatima Zahra Mernissi i Inçaf Mokhtar j Raouf Dahoui k Mohamed Denguezli l Nejib Doss k Hamida Turki m a Department of Dermatology, CHU Mustapha, and b Department of Dermatology, CHU Bab El Oued, University of Algiers, Algiers , c Department of Dermatology, EHS Oran, University of Oran, Oran , and d Department of Dermatology, CHU Annaba, University of Annaba, Annaba , Algeria; e Department of Dermatology, CHU Ibn Rochd, Casablanca , f Department of Dermatology, CHU Mohammed V., Marrakesh , g Department of Dermatology, CHU Ibn Sina, and h Department of Dermatology, Cheikh Zaid Hospital, Rabat , and i Department of Dermatology, CHU Hassan II, Fes , Morocco; j Department of Dermatology, Habib Thameur Hospital, and k Department of Dermatology, Military Hospital of Instruction of Tunis, Tunis , l Department of Dermatology, CHU Farhat Hached, Sousse , and m Department of Dermatology, CHU Hedi Chaker, Sfax , Tunisia
Abstract
Background: Psoriasis is a common skin disorder that is characterized by red plaques covered with silvery scales and is associated with considerable psychosocial impact. It has been described in several studies worldwide, but specific data from the Maghreb (Algeria, Morocco and Tunisia) are
unavailable. Objectives: To characterize the frequency of new psoriasis cases and to describe the epidemiological and clinical profile of psoriasis in the Maghreb. Methods: A psoriasis
working group for the Maghreb initiated the EPIMAG international multicentre cross-sectional observational epidemiological study coupled with a 2-week psoriasis screening study via medical consultation. Data were collected via questionnaires. Results: The total analysis population included 373 pre-existing and 326 new psoriasis cases, described by 261 participating investigators. The frequency of new psoriasis cases was 10.26/1,000 in Algeria, 15.04/1,000 in Morocco and 13.26/1,000 in Tunisia, and thus 12.08/1,000 in the Maghreb. In all 699 psoriasis subjects, the mean age was 46 years, the mean BMI was 26.6, and 55.7% of subjects were men. Two thirds of the subjects had never smoked, and 85.0% had never consumed alcohol. Half had brown skin, and 28.6% had a family history of psoriasis. Three quartershad localized psoriasis, 85.8% had plaque psoriasis, coupled with pruritus in over 70.0% of cases. Flares or outbreaks were most often triggered by stress (79.4%) and change of season (43.1%). The majority of subjects used topical therapy, and the investigators considered overall treatment efficacy to be partial in over half of the cases. Among patients with preexisting psoriasis, secondary analyses showed that 73.2% had severe psoriasis, and that quality of life was severely affected in 40.1% of cases. The mean number of missing school or work days over 6 months was 3.2 (±12.1) days.
Conclusions:
Our study provides novel information relative to psoriasis epidemiology and characterization in the Maghreb and highlights the need to improve psoriasis screening and management in the region. The data will help optimize psoriasis management, to ensure appropriate national health care policies.
Introduction
Psoriasis is a chronic inflammatory non-infectious and non-contagious skin disorder. Classic psoriasis manifests as well-demarcated red plaques covered with silvery scales, usually localized to the shoulders, knees and scalp. Various pustular forms have also been identified, and symptoms may also include articular inflammation in the case of psoriatic arthritis [1, 2] . Psoriasis development is influenced by environmental and genetic factors, and family history [3–5] .
Although severe physiological consequences are rare, the psychosocial impact on health-related quality of life (QoL) is considerable, and not limited to severe psoriasis [6] . The American National Psoriasis Foundation (NPF) reported that 71% of patients claimed their psoriasis had a moderate-to-severe effect on QoL, affecting everyday life. Psoriasis causes emotional stress, impaired self-esteem and depression [7, 8] , increasing the disease’s psychological burden. A recent Algerian study showed that over three quarters of patients with psoriasis considered their QoL affected, and that the disease was a major handicap in 6.8% of cases [9] .
Psoriasis is common and has been the focus of multiple studies worldwide. However, specific data from the Maghreb (Algeria, Morocco and Tunisia) are unavailable.
Epidemiological studies conducted so far in the region have mainly been retrospective single-centre hospital studies [9–13] . Psoriasis prevalence has been estimated at 2.3% in Morocco [12] and 3.0% in Tunisia [3] , consistent with estimates reported in other countries [14] .
A psoriasis working group for the Maghreb, composed of 14 dermatologists, was created in 2010. The
group initiated discussion and action in order to optimize psoriasis management and improve psoriasis characterization in the Maghreb. The PSOMAG cross-sectional study on the frequency of psoriasis seen by general practitioners (GPs) and dermatologists was the first to be initiated by this working group [15].
The EPIMAG (‘Epidemiological and clinical profile of psoriasis patients followed by GPs and dermatologists in the Maghreb and systematic screening over a 2-week period’) international multicentre cross-sectional observational epidemiological study followed. The EPIMAG is the first such
study in the Maghreb characterizing the frequency of new psoriasis cases and describing epidemiological and clinical profiles of these cases. It provides clinical and epidemiological characterization of patients with psoriasis in the Maghreb coupled with psoriasis screening via medical consultation.
Methods
Study Design
International cross-sectional epidemiological observational study characterizing psoriasis coupled with a 2-week psoriasis screening study via medical consultation, conducted in Algeria, Morocco and Tunisia.
Setting
Approvals were obtained from each participating country,from the CCTIRS on December 15, 2011, and from the CNIL on March 20, 2012. Questionnaires were completed between March 13, 2012, and August 12, 2012. Data quality control was carried out by BIOSTATEM during the data management phase, which had a cutoff date of August 31, 2012. Investigators who agreed to participate in the study received a contract by mail with questionnaires for psoriasis characterization and diagnosis, along with envelopes for the completed questionnaires and signed contracts to be returned. The GPs and dermatologists contacted to participate in this study belong to a representative sample of health care professionals previously recruited in the PSOMAG study [15] . The number of recruiting GPs was calculated as a function of the medical demographics of each country. GPs were chosen randomly in each country, stratified by regions, and 20 dermatologists per country were also recruited.
Data Collection
Data were collected via two similar questionnaires that contained additional questions adapted to the characteristics of the patient groups with existing or newly diagnosed disease. Investigators recorded psoriasis management data and clinical characterization of existing psoriasis cases (EPIMAG1). Patients were included in chronological order of consultations over a period of 2 months. Investigators completed a medical history questionnaire for each patient, including demographic data, date of diagnosis, clinical data (e.g. medical history, psoriasis evaluation), QoL data, and missing school or work days. As part of the systematic screening of new psoriasis cases (EPIMAG2), investigator data, date of diagnosis and
clinical data were collected. At the study end, the total number of patients seen in consultation and the number of patients diagnosed during the 2-week screening period were collected for each centre.
Systematic psoriasis screening was implemented following a common training programme developed by the working group and taught by panel members during conferences for the benefit of the participating GPs. Completion of this training was a condition for GP participation in EPIMAG2. Screening was conducted by GPs and dermatologists on subjects’ elbows, knees and scalps without affecting the usual medical practice. A questionnaire was completed for each newly diagnosed case, and the patient was
treated as per usual practice.
Participants
In the EPIMAG1, adult patients with previously diagnosed psoriasis and followed for psoriasis were included. In the EPIMAG2, eligibility criteria included all adult patients seen in consultation over a 2-week period willing to participate in the study after being informed.
Variables
Variables generated from questionnaires included age, date of diagnosis, body mass index (BMI), severity of known cases, psoriasis type (generalized, localized and/or erythrodermic), and other
manifestations (rheumatism, peripheral, axial or mixed involvement).
In the QoL evaluation by investigators, if at least 1 QoL item was assessed as ‘incapacitating’, psoriasis was considered severe.
Psoriasis is considered severe if it requires systemic treatment, is generalized or affects >20% of the total body surface, if it is local with pustular and/or erythrodermic lesions, or if it is associated with other manifestations (rheumatism, peripheral involvement, axial and/or mixed) [16] . The frequency of new psoriasis cases was calculated by dividing the number of psoriasis cases diagnosed with the total number of patients who consulted during the 2 weeks of screening. In the secondary analysis, the percentage of patients with severe psoriasis was described. Missing psoriasis severity data was completed by taking into account large alterations of QoL, and the number of missing work or school days over 6 months for each known psoriasis case.
Study Size
The number of participating centres was calculated in the previous PSOMAG study for a frequency estimate with a 1/1,000 precision [15] . Medical and population demographic data per country
were used in the calculation. Differences in the number of recruited GPs between countries reflect the different numbers of practising health care professionals. In order to describe the different variables across the Maghreb, between 100 and 200 pre-existing psoriasis cases per country were sufficient. Recruitment was divided between GPs and dermatologists. Based on the PSOMAG, 2 pre-existing psoriasis cases could be described per GP in a 2-month period. Four patients were described by each dermatologist. A total of 410 pre-existing psoriasis cases needed recruiting by GPs and 240 cases by dermatologists.
Bias
To minimize potential selection bias, training programmes were done for GPs, and biased psoriasis data were reviewed by the scientific committee.
The severe psoriasis types are: palmoplantar keratosis, non-responder psoriasis, generalized psoriasis excluding erythroderma,psoriasis with a psychological and social impact.
The psoriasis severity was not measured by the PASI scale because it was not adequate for GPs who represented the most important investigators participating in this trial, so therefore it was removed from the questionnaire of psoriasis severity assessment.
Statistical Methods
Data are presented for the region as a whole; no statistical comparisons between countries were performed. Epidemiological and clinical characterization of patients with psoriasis was done
through descriptive analyses of the collected variables. The distribution of quantitative variables was described by frequency, means, standard deviations, medians and ranges. Qualitative variables
were described by frequency and by the percentage of patients in each category. Missing data were not included in calculating percentages. The upper 95% confidence intervals were estimated in the primary analysis. Statistical analyses were performed with SAS ® software (version 9.3). Duplicate interactive data capture was performed using Clinsight ® software (version 6.2). The accepted error rate was 1% for all data.
Results
Participants
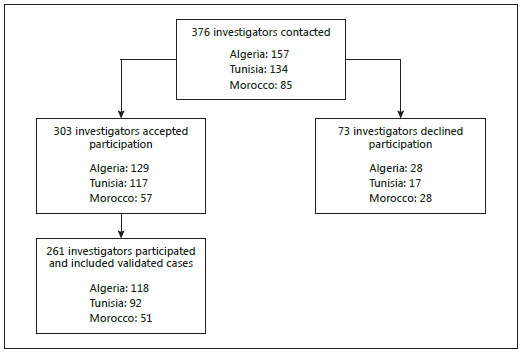
Overall, 376 investigators were contacted: 157 in Algeria, 134 in Tunisia and 85 in Morocco. Among these, 73 declined participation ( fig. 1 ) for the following reasons: too many other professional obligations; absent during the screening period; unable or unwilling to contact patients; did not frequently see psoriatic patients; difficulties in recruiting patients (e.g. for geographic reasons,
or because informed consent was refused). In total, 303 investigators (80.6%) accepted participation in the study ( fig. 1 ). Among these, 261 investigators (69.4%) participated in the EPIMAG (recruited validated cases), including 118 in Algeria, 92 in Tunisia and 51 in Morocco.
Among participating investigators, 172 (65.9%) completed at least 1 questionnaire describing pre-existing cases (EPIMAG1), and 194 (74.3%) participated in the screening study (EPIMAG2). Within the latter group, 131 (67.5%) diagnosed at least 1 new psoriasis case. The majority of investigators worked in private practices (91.9 and 76.8% for EPIMAG1 and EPIMAG2, respectively) and were GPs in 78.5 and 82.0% of cases for the EPIMAG1 and EPIMAG2, respectively.
In total, investigators included 753 psoriasis cases (396 pre-existing and 357 new cases). Among these, 54 were minors and were excluded. The analysis population thus included 699 subjects (92.8%), 261 of whom consulted in Algeria, 171 in Morocco and 267 in Tunisia. Of the 699 subjects, 373 were pre-existing cases (EPIMAG1) and 326 were new cases (EPIMAG2).
Demographic Data and Analysis of Primary
Objectives
Overall, subjects had a mean age of 46 years (range, 18–92 years), and 55.7% were men; the proportion of male patients was especially elevated in Morocco (57.3%) and Tunisia (61.0%). The average height was 1.68 m for an average 75.6 kg weight, and a mean BMI of 26.6. The mean waist circumference was 91.9 cm. In all, 15.5% of subjects were current and regular smokers, 63.9% had never smoked, 1.6% were regular alcohol users, and 85.0% had never consumed alcohol. Half of the subjects (51.1%) had brown skin, and 28.6% had a family history of psoriasis ( table 1 ). Finally, 19.7 and 17.7% had current or ongoing atopy and diabetes, respectively.
Clinical data showed that 75.2% had localized psoriasis, 85.8% had plaque psoriasis, coupled with pruritus in over 70.0% of cases. Other symptoms were recorded in 19.7% of cases, including rheumatic manifestations (81.9%) or peripheral involvement (27.5%). Psoriasis evolution was progressive in 25.2% of subjects. Flareups or outbreaks were triggered by stress in almost 80% of subjects, followed by change of season in 43.1% of subjects and weight increase in 12.4% of cases ( table 2 ).
Psoriasis medical history was described in all known cases. Psoriasis was diagnosed on average approximately 10 years previously. 97.3% of subjects used topical ther apy, and 33% used systemic treatment. In about half of the cases (52.4%), overall efficacy of treatment was considered partial by the clinician ( table 3 ). In subjects with pre-existing psoriasis, the most affected zones were the legs (76.7% on either side from the front) and arms (65.1% on the right and 66.5% on the left, from the back,
table 4 ). To increase patient acceptability of the systematic psoriasis screening part of the study (EPIMAG2), psoriasis location was simply recorded on the subject’s elbows, knees and scalp, without affecting the usual medical practice. Among these newly diagnosed cases, almost half had psoriasis on the elbows or knees (49.1 and 46.6%, respectively), and 36.2% of the subjects had psoriasis on
the scalp.
The frequency of new psoriasis cases measured during the 2-week screening period ( table 5 ) was 10.26/1,000 in Algeria, 15.04/1,000 in Morocco and 13.26/1,000 in Tunisia. In the Maghreb region overall, psoriasis frequency of newly diagnosed cases was estimated at 12.08/1,000.
Secondary Analyses
Among the 373 patients with pre-existing psoriasis, investigators assessed that 73.2% had severe psoriasis, and that QoL was severely affected in 40.1% of cases, either on a professional or social level. Everyday life was moderately-to-severely affected by psoriasis in 32.1% of cases, professional activities in 25.4% of cases and social relationships in 28.6% of cases. Treatment side effects moderately-to-severely
affected 10.4% of patients, and 13.2% answered that psoriasis interfered with their education.
When including mildly affected patients, psoriasis affected everyday life, professional activities and social relationships in 57.7, 43.5 and 51.2% of cases, respectively.
The mean number of missing school or work days over 6 months was 3.2 (±12.1) days.
Discussion
EPIMAG provides an epidemiological and clinical profile of psoriasis and determines the frequency of newly diagnosed psoriasis cases in the Maghreb. It is the first multicentre study of its kind in the region and is important because psoriasis clinical characteristics are known to vary between populations and regions [17] .
Study participation rates were elevated. Of the investigators participating in EPIMAG, 172 (65.9%) completed at least one questionnaire describing pre-existing cases (EPIMAG1), and 194 (74.3%) participated in the screening study (EPIMAG2). The majority were GPs working in private practices. The analysis population comprised 699 subjects, including 373 with pre-existing psoriasis (EPIMAG1) and 326 new cases (EPIMAG2).
The patients with psoriasis who agreed to participate were relatively young (average age of 46 years), tended to be men (56%) and had a mean BMI of 26.6 (overweight according to WHO reference values). Psoriasis is known to affect both genders in equal measure[18] . The overrepresentation of male patients in Morocco and Tunisia may be explained by the social context, whereby women have more limited access to health care[19, 20] , and fewer women are medical professionals[21] .
The majority of subjects were non-smokers (63.9%) and had never consumed alcohol (85.0%). Lifestyle choices such as smoking or alcohol consumption are known psoriasis risk factors[22] ; given the social and religious context in the Maghreb region, responses to questions about tobacco and alcohol consumption should be interpreted with caution. Obesity and smoking may increase the risk of developing psoriasis[23, 24] . Patients with psoriasis are more likely to be obese compared with the general population[25]. Diabetes was recorded in 17.7% of subjects and
was associated with psoriasis duration and severity, and not necessarily driven by elevated BMI alone[26, 27] .
Although it has been suggested that Caucasians are more frequently affected by psoriasis than other populations[14,28] , there were no significant differences between skin types. About a third of subjects had a family history of psoriasis, similar to rates from other countries [29] .
Three quarters of subjects (75.2%) had localized psoriasis, 85.8% had plaque psoriasis, coupled with pruritus in over 70% of cases. Other symptoms were recorded in 19.7% of cases, including rheumatic manifestations.
Frontally, psoriasis was most often localized to the legs, whereas from the back, psoriasis was most often localized to the arms. Data on the percentage body area affected reflect other studies[30] ; most patients with psoriasis have limited disease affecting less than one palm-sized area[31] .
Psoriasis was diagnosed approximately 10 years earlier.
Among subjects with pre-existing psoriasis, 97.3% used topical therapy and 33% used systemic treatment, similar to data reported in European studies[32, 33] .
However, the study was not designed to compare the efficacy of different treatments. Importantly, the EPIMAG observed that overall treatment efficacy was considered partial in 52.4% of cases, confirming that there is room for improving psoriasis management in the Maghreb.
Psoriasis flares were triggered by stress in almost 80% of subjects, again reflecting data from studies conducted worldwide. Stress is described as a key disease trigger in up to 60% of patients[29, 34–36] . Change of season and weight increase were noted as triggering flares in 43.1 and 12.4% of subjects, respectively. Psoriasis prevalence has been shown to be more common in colder climates than
in tropical regions[17] , and patients who gain weight have been reported to respond less well to treatment[37] .
The previous PSOMAG study estimated a low psoriasis frequency detected by GPs and dermatologists in the Maghreb (2.3/1,000; 95% confidence interval, 1.8/1,000–2.8/1,000), which was mainly attributed to the limited number of dermatologists in the Maghreb compared with the population, and to poor awareness of disease pathology[15]. GP awareness was thus increased with a screening training programme included in the EPIMAG study.
The PSOMAG highlighted that most patients with psoriasis (up to 90%) were likely not followed or diagnosed.
The EPIMAG screening study estimated a fivefold higher psoriasis frequency in the Maghreb following GP training (12.08/1,000), confirming the hypothesis highlighted in the PSOMAG study. These new psoriasis frequency estimates remain well below the recorded ‘true’ estimated prevalence. Psoriasis prevalence in the Maghreb has been estimated between 2.3 and 3.0%[3, 12] . In Europe, psoriasis
prevalence estimates vary from 0.6 to 6.5%[14] . In the USA, approximately 2.0% of the population is affected, and the estimated prevalence of diagnosed psoriasis is 3.15%[38] . The psoriasis frequency rates detected by GPs and dermatologists in the Maghreb in the PSOMAG and EPIMAG studies confirm that the majority of psoriasis cases are not followed or diagnosed, and that the GP training programme had a strong impact on psoriasis screening.
Secondary analyses showed that investigators assessed almost three quarters (73.2%) of known psoriasis cases as severe. This proportion is higher than European surveys, in which moderate-to-severe psoriasis was confirmed by dermatologists in 79.3% of patients[39] , and 74% of participating subjects considered their psoriasis as at least moderately severe[32] . In the absence of rigorous data enabling the characterization of psoriasis severity (apart from the PASI), classification of severe psoriasis was
mostly recoded by study working group members, which may have led to bias.
Among pre-existing psoriasis cases, QoL was severely affected in 40.1% of cases, either on a professional or social level. When counting all affected patients (including those mildly affected), approximately half had disease affecting everyday life, professional activities and social relationships.
Psoriasis adversely affected physical activity and social relationships in ≥ 50% of 330 Kuwaiti patients,
as measured by the patient-generated dermatology QoL scale[40] . In another patient questionnaire study, psoriasis affected overall emotional well-being in 88% of patients and enjoyment of life in 82% of patients[41] . An NPF survey found that 71% of patients considered psoriasis a significant issue in everyday life. Around 35% of patients avoided social activities, dating or intimate relationships[7].
The mean number of missing school or work days reported in the EPIMAG (3.2 ± 12.1 over a 6-month period) is lower than those of other studies. An Algerian study estimated this figure at 15 days/year. In a typical month, an NPF survey found that, among employed respondents who missed work days due to psoriasis, 62% missed 5 days or less, 6.6% missed 6–10 days, and 31% missed >10= days; 49% missed work days regularly[41] . The negative impact of psoriasis on professional life and work productivity
is undeniable[42] .
The EPIMAG is limited by the fact that it does not provide an exhaustive picture, due to the limited sample size and to difficulties in including patients from remote areas.
However, strong trends were observed. Although the representativeness of the sample and the quality of the responses provided cannot be verified in detail, acceptance and participation rates were elevated. In addition, small variations in psoriasis evaluation depending on whether the case was pre-existing or newly diagnosed may have biased the uniform description of all psoriasis cases.
In conclusion, the EPIMAG provides new psoriasis epidemiological information, highlights the efficacy and impact of psoriasis screening training and improves the characterization of psoriasis in the Maghreb. Future research may benefit from long-term observational studies with larger patient samples. The EPIMAG demonstrates that a large majority of psoriasis cases are not followed or diagnosed, despite the strong impact of psoriasis on QoL. It is necessary to improve psoriasis screening and management
in the Maghreb. From a public health perspective, it is important to collect data on psoriasis frequency,
burden and management, to ensure appropriate national health care policies.
Acknowledgements
We thank Dr. Vanessa Gray-Schopfer, OmniScience SA, and Springer who provided medical writing services. The authors were fully responsible for the contents of and editorial decisions for this paper. Funding was provided by an unconditional grant of LEO Pharma.
Disclosure Statement
The experts declare no conflict of interest.
References
1 Langley RG, Krueger GG, Griffiths CE: Psoriasis:
epidemiology, clinical features, and quality of life. Ann Rheum Dis 2005;64(suppl 2): ii18–ii23, discussion ii4–ii5.
2 Schon MP, Boehncke WH, Brocker EB: Psoriasis: clinical manifestations, pathogenesis
and therapeutic perspectives. Discov Med 2005;5:253–258.
3 Ammar M, Zaraa I, Bouchleka Souissi C, Dhaoui A, Doss N, Ben Osman A, et al: Familial psoriasis: descriptive report of 9 families (in French). Tunis Med 2009;87:750–754.
4 Dereure O, Guilhou JJ: Epidemiology and genetics of psoriasis (in French). Ann Dermatol Venereol 2003;130:829–836.
5 Guinot C, Latreille J, Perrussel M, Doss N, Dubertret L: Psoriasis: characterization of six different clinical phenotypes. Exp Dermatol 2009;18:712–719.
6 Rapp SR, Feldman SR, Exum ML, Fleischer AB Jr, Reboussin DM: Psoriasis causes as much disability as other major medical diseases. J Am Acad Dermatol 1999;41:401–407.
7 National Psoriasis Foundation 2008 survey panel snapshot. http://www.psoriasis.org/ document.doc?id=193 (accessed January 23, 2013).
8 Evers AW, Lu Y, Duller P, van der Valk PG, Kraaimaat FW, van de Kerkhof PC: Common burden of chronic skin diseases? Contributors to psychological distress in adults with psoriasis and atopic dermatitis. Br J Dermatol 2005; 152:1275–1281.
9 Boudaya S, Turki H, Marrakchi S, Meziou TJ, Bouassida S, Zahaf A: Le psoriasis de l’enfant: étude épidémiologique de 196 observations. Nouv Dermatol 2004;23:13–16.
10 Daoud L, Dhaoui MR, Youssef S, Jaber K, Doss N: Management of severe psoriasis: about 50 cases (in French). Tunis Med 2007; 85:849–856.
11 Jalal O, Houass S, Laissaoui K, Hocar O, Charioui S, Amal S: Severe psoriasis: 160 cases (in French). Ann Dermatol Venereol 2005;132: 126–128.
12 Skali S, Berrada R, Benchikhi H, Lakhdar H: Profil épidémiologique du psoriasis au service de dermatologie de Casablanca. Etude de 3,021 cas. Nouv Dermatol 2009;28:427–430.
13 Zaara SY, Mrabet A, Jaber K, Ketaeri I, Ben Mna A, Amri A, et al: Epidemiology of severe non-infectious skin diseases of foot among soldiers: a study of 128 inpatient cases. Rev Tunisienne Santé Milit 2010;12:184–188.
14 Chandran V, Raychaudhuri SP: Geoepidemiology and environmental factors of psoriasis and psoriatic arthritis. J Autoimmun 2010; 34:J314–J321.
15 Benchikhi H, Amal S, Ammar-Khodja A, Benkaidali I, Bouadjar B, Dhaoui M, et al: Étude PSOMAG: prévalence des cas de psoriasis au Maghreb (abstract P097). Ann Dermatol Vénéréol 2012;139:B162–B163.
16 Guideline on clinical investigation of medicinal products indicated for the treatment of psoriasis. EMEA/CHMP/EWP/2454/02. London, November 18, 2004.
17 Christophers E: Psoriasis – epidemiology and clinical spectrum. Clin Exp Dermatol 2001; 26:314–320.
18 Gelfand JM, Weinstein R, Porter SB, Neimann AL, Berlin JA, Margolis DJ: Prevalence and treatment of psoriasis in the United Kingdom: a population-based study. Arch Dermatol 2005;141:1537–1541.
19 World Health Organization: Country cooperation strategy at a glance: Tunisia. http:// www.who.int/countryfocus/cooperation_ strategy/ccsbrief_tun_en.pdf. 2006 (accessed January 23, 2013).
20 Semlali H: The global health workforce alliance. Positive practice environments in Morocco. http://www.who.int/workforcealliance/ knowledge/PPE_Morocco_CaseStudy.pdf. 2010 (accessed January 23, 2013).
21 Aounallah-Skhiri H, Lazaar-Ben Gobrane H, Hsairi M, Achour N, Zouari B, Nacef T: Medical demography in Tunisia: current situation and perspectives (in French). Tunis Med 2012;90:166–171.
22 De la Brassinne M, Failla V, Nikkels A: Psoriasis: state of the art 2013. Acta Clin Belg 2013;68:427–432.
23 Naldi L, Chatenoud L, Linder D, Belloni Fortina A, Peserico A, Virgili AR, et al: Cigarette smoking, body mass index, and stressful life events as risk factors for psoriasis: results from an Italian case-control study. J Invest Dermatol 2005;125:61–67.
24 Setty AR, Curhan G, Choi HK: Obesity, waist circumference, weight change, and the risk of psoriasis in women: Nurses’ Health Study II. Arch Intern Med 2007;167:1670–1675.
25 Armstrong AW, Harskamp CT, Armstrong EJ: The association between psoriasis and obesity: a systematic review and meta-analysis of observational studies. Nutr Diabetes 2012;2:e54.
26 Armstrong AW, Harskamp CT, Armstrong EJ: Psoriasis and the risk of diabetes mellitus: a systematic review and meta-analysis. JAMA Dermatol 2013;149:84–91.
27 Brauchli YB, Jick SS, Meier CR: Psoriasis and the risk of incident diabetes mellitus: a population-based study. Br J Dermatol 2008;159: 1331–1337.
28 Gelfand JM, Stern RS, Nijsten T, Feldman SR, Thomas J, Kist J, et al: The prevalence of psoriasis
in African Americans: results from a population-based study. J Am Acad Dermatol 2005;52:23–26.
29 Rigopoulos D, Gregoriou S, Katrinaki A, Korfitis C, Larios G, Stamou C, et al: Characteristics
of psoriasis in Greece: an epidemiological study of a population in a sunny Mediterranean climate. Eur J Dermatol 2010;20: 189–195.
30 Valenzuela F, Silva P, Valdes MP, Papp K: Epidemiology and quality of life of patients with psoriasis in Chile. Actas Dermosifiliogr 2011; 102:810–816.
31 Stern RS, Nijsten T, Feldman SR, Margolis DJ, Rolstad T: Psoriasis is common, carries a substantial
burden even when not extensive, and is associated with widespread treatment dissatisfaction. J Investig Dermatol Symp Proc 2004;9:136–139.
32 Fouere S, Adjadj L, Pawin H: How patients experience psoriasis: results from a European survey. J Eur Acad Dermatol Venereol 2005; 19(suppl 3):2–6.
33 Vena GA, Altomare G, Ayala F, Berardesca E, Calzavara-Pinton P, Chimenti S, et al: Incidence of psoriasis and association with comorbidities in Italy: a 5-year observational study from a national primary care database. Eur J Dermatol 2010;20:593–598.
34 Farber EM, Nall ML: The natural history of psoriasis in 5,600 patients. Dermatologica 1974;148:1–18.
35 Seville RH: Psoriasis and stress. Br J Dermatol 1977;97:297–302.
36 Fortune DG, Richards HL, Main CJ, Griffiths CE: What patients with psoriasis believe about their condition. J Am Acad Dermatol 1998;39:196–201.
37 Bardazzi F, Balestri R, Baldi E, Antonucci A, De Tommaso S, Patrizi A: Correlation between BMI and PASI in patients affected by moderate to severe psoriasis undergoing biological therapy. Dermatol Ther 2010;23(suppl 1):S14–S19.
38 Kurd SK, Gelfand JM: The prevalence of previously diagnosed and undiagnosed psoriasis in US adults: results from NHANES 2003– 2004. J Am Acad Dermatol 2009;60:218–224.
39 Garcia-Diez A, Foraster CF, Sebastian FV, Tudela LL, Llach XB, Fernandez GS: What characterizes the severity of psoriasis? Results from an epidemiological study of over 3,300 patients in the Iberian region. Dermatology 2008;216:137–151.
40 Al-Mazeedi K, El-Shazly M, Al-Ajmi HS: Impact of psoriasis on quality of life in Kuwait. Int J Dermatol 2006;45:418–424.
41 Armstrong AW, Schupp C, Wu J, Bebo B: Quality of life and work productivity impairment among psoriasis patients: findings from the National Psoriasis Foundation survey data 2003–2011. PLoS One 2012;7:e52935.
42 Pearce DJ, Singh S, Balkrishnan R, Kulkarni A, Fleischer AB, Feldman SR: The negative impact of psoriasis on the workplace. J Dermatolog Treat 2006;17:24–28.